
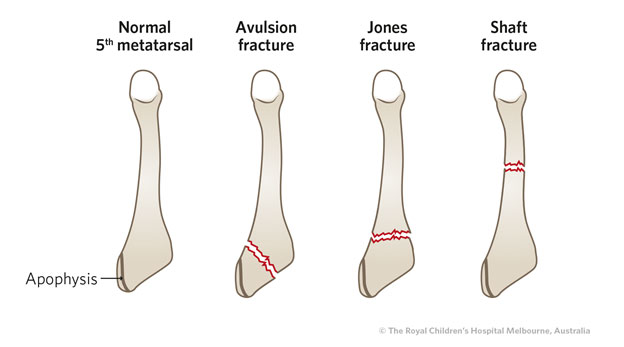
Rosenberg shared a similar opinion in his review paper on treatment for zone 2 and 3 fractures ( 24). Among the recruited 37 patients (18 patients with casting and 19 patients with screw fixation), he observed that non-operative treatment causes a relatively high rate of treatment failure (44%) and doubles the time to clinical union and return to sports. Mologne performed the only randomized controlled study comparing the outcome of early intramedullary screw fixation versus casting for Type I fractures ( 23). C, radiograph taken 15 months after the injury, showed the notch disappeared. The notch is a common radiographic appearance after the fracture heals. B, radiograph taken nine weeks after the injury showed that the fracture healed with residual lateral cortical notch. However, another study showed that functional treatment in this group of fractures gives good results compared to non-displaced and extra-articular fractures ( 15) ( Figure 3).Ī Case of Lawrence and Botte Zone 3 Fracture Treated Conservatively With a CastĪ, injury film. Some authors suggested that fracture displacement of more than 2 cm and involvement of more than 30% of the cuboid-metatarsal articulation are indications for operative treatment of tuberosity avulsions ( 8). Therefore, functional treatments with orthopedic shoe, Jones bandage dressing or elastic bandage dressing are recommended. However, studies have shown that functional treatments with early weight bearing provide better functional outcome and earlier return to work than treatment by short leg cast with non-weight bearing walking ( 18- 21). A meta-analysis of 187 tuberosity avulsion fractures from four studies in 2011 showed that there was no significant difference in union and refracture rates between different conservative treatment modalities ( 17). There is no controversy that non-displaced tuberosity avulsion fractures should be treated conservatively in view of their excellent healing potential. Complications of these fractures and their management are discussed in this report. For cases presented with signs of delayed union and non-union, surgical treatment with or without bone grafting is recommended. Therefore, early surgical fixation with intramedullary screw is advised in athletic individuals. For zone 2 and zone 3 fractures, acute forms can be treated conservatively but with a risk of delayed union time and time for return to function. Zone 1 fractures are treated conservatively with functional immobilization and early mobilization with excellent outcome. Lawrence and Botte classify proximal fifth metatarsal fractures according to their location: tuberosity avulsion fractures (zone 1), fractures at metaphyseal-diaphyseal junction extending into the fourth-fifth intermetatarsal joint (zone 2) and proximal diaphyseal fractures (zone 3). The radiographic classification that we have proposed is intended to aid surgeons treating and discussing fractures localized to the distal portion of the fifth metatarsal.ĭiagnosis diaphysis injury radiograph tent sign trauma.The vascular supply and soft tissue anatomy of the fifth metatarsal explains the increased risk of delayed union and non-union in fractures at the metaphyseal-diaphyseal junction. To our knowledge, a classification system for fractures of the distal shaft of the fifth metatarsal has not been previously reported. Grade I and III fractures accounted for 29% and 22% of the distal fifth metatarsal fractures, respectively. Grade II fractures were most prevalent and accounted for 49% of the cases reviewed. Four distinct fracture configurations emerged as a result of our radiographic analysis, and these were categorized as grades I, IIA, IIB, and III. The sample was grouped into "grades" of deformity according to the configuration of the fracture and the amount of displacement observed for each injury. The classification system is based on a review of 79 spiral oblique fractures of the distal shaft of the fifth metatarsal. In the present report, a new radiographic classification for distal shaft fractures of the fifth metatarsal is presented.


 0 kommentar(er)
0 kommentar(er)
